Guidelines on the Management of Patients with Vestibular Schwannoma
1. Introduction and Methods
download pdf Neurosurgery, 2017
Sponsored by: Congress of Neurological Surgeons (CNS) and the AANS/CNS Tumor Section
Endorsed by: Joint Guidelines Committee of the American Association of Neurological Surgeons (AANS) and the Congress of Neurological Surgeons (CNS)
Jeffrey J. Olson, MD11, Steven N. Kalkanis, MD2, Timothy C. Ryken, MD3
1. Department of Neurosurgery, Emory University School of Medicine, Atlanta, Georgia, USA
2. Department of Neurosurgery, Henry Ford Health System, Detroit, Michigan, USA
3. Department of Neurosurgery, Dartmouth University School of Medicine, Hanover, New Hampshire, USA
Correspondence:
Jeffrey J. Olson, MD
Department of Neurosurgery
Emory University School of Medicine
Atlanta, Georgia
Email: jolson@emory.edu
Disclaimer of Liability
This clinical systematic review and evidence-based guideline was developed by a physician volunteer task force as an educational tool that reflects the current state of knowledge at the time of completion. Each chapter is designed to provide an accurate review of the subject matter covered. This guideline is disseminated with the understanding that the recommendations by the authors and consultants who have collaborated in their development are not meant to replace the individualized care and treatment advice from a patient's physician(s). If medical advice or assistance is required, the services of a competent physician should be sought. The proposals contained in these guidelines may not be suitable for use in all circumstances. The choice to implement any particular recommendation contained in these guidelines must be made by a managing physician in light of the situation in each particular patient and on the basis of existing resources.
Background and Rationale
Vestibular schwannomas (VS) are uncommon lesions that are a substantial challenge to the neurosurgeons and otologists who undertake their clinical management. The majority of the population may live their entire lives without ever hearing the term VS, let alone knowing an affected individual. To provide context, only approximately 3300 VSs are diagnosed per year in the United States, indicating an incidence of 1.09 per 100,000 people. This incidence increases with age, peaking in the 65- to 74-year-old age group. The incidence is higher in Asian Pacific Islanders and lower in African Americans and Hispanics.1 Based on a 2010 study, the estimated prevalence (1:60,000) is higher than previously believed.2 An important subset of these individuals also have neurofibromatosis type 2 (NF2), potentially allowing a basis on which to understand the underlying molecular genesis of these lesions.2-5
The treatment goals for any cranial neoplasm, whether benign or malignant, are either disease cure or meaningful control, along with maintenance of neurologic function and quality of life. The presence of a VS has been associated with a decline in health-related quality of life measurement, regardless of the management chosen, including observation alone. Interestingly, microsurgical management has been associated with the greatest decrement in health-related quality of life measurements. Patients who underwent microsurgery had statistically significantly worse outcomes in their Pennsylvania Acoustic Neuroma Quality of Life total score by 8% to 11% (P < .023) compared with those treated with stereotactic radiosurgery or observation, respectively. The scores for those undergoing microsurgery were significantly less (P < .001) than those treated with stereotactic radiosurgery or observation in the subdomains of facial function (13–14%), balance (10–19%), and pain (19–30%). These findings must be balanced against more patients with unequivocal tumor growth or intractable symptoms having undergone microsurgical intervention.6 This may not be surprising to many surgeons, and the history of the surgical management of these lesions is replete with valiant attempts at improvement.
One of the earliest documented attempt at surgical resection of a VS via a unilateral suboccipital approach was noted by Annandale in 1895.7 Early surgery in the cerebellopontine angle region has been limited by technical ability, equipment, anesthesia, and late presentation. Even Cushing referred to this location as the “bloody angle,” although he substantially improved outcomes in the 1920s compared with his surgical predecessors.8,9 By the 1940s, Dandy had reduced the mortality rate to just over 10%, advocating total resection over intracapsular removal as advocated by Cushing.10-13 Middle fossa approaches for various syndromes of the vestibulocochlear complex have been reported since at least 1904 when Parry described the approach, attempting surgical management for tinnitus.14 The first translabyrinthine VS resection was reported as part of a 2-stage procedure by Franciscus H. Quix in 1912.15 This approach was popularized by William House, and along with the retrosigmoid approach, have become the mainstay of surgical management of VS.16
In the modern era, the development of alternatives to surgical management have become important considerations in the discussion of VS therapy. For example, the original description of stereotactic radiosurgery (Gamma Knife) by Leksell17,18 did not specifically envision treatment of VS; however, these lesions have become an appealing target for this minimally invasive option. In addition, although generally applied to malignant disease, bevacizumab has been suggested as a possible therapy in select cases of NF2, adding the consideration of medical therapy to the discussion of VS management options.19
Outcomes remain imperfect, and improvements in these therapeutic steps are necessary. This is as true for surgical management as it is for radiotherapy approaches.20-22 Although much information has been garnered from current large retrospective clinical data series, it appears we have maximized the information to be gained by simply increasing the numbers of patients treated in the same fashion and adding to the duration of follow-up.
The population of patients with VSs is a heterogeneous one with differences in age at presentation, baseline hearing and neurologic status, overall health, tumor size and location, and patient preferences and biases. Outcome is not a singular entity either and can be measured by extent of resection, postoperative hearing and neurologic status, period of disease control, and type of therapy needed for management of recurrence. A matrix of decision nodes for an algorithm or decision tree addressing these items in a meaningful fashion is not achievable. First, because of its obvious complexity and secondarily because of the class III or lack of data addressing many of those decisions. A useful starting point to improving the current knowledgebase is to define the benchmarks of our current knowledge regarding VS management using evidence-based techniques in order to allow meaningful points of departure for future scientific and clinical research.
Objectives and Guideline Panel Development
Recognizing the important health impacts of VSs, along with the lack of consensus among various treatment options, the Joint Tumor Section of the American Association of Neurological Surgeons (AANS) and the Congress of Neurological Surgeons (CNS) recommended that evidence-based guidelines be developed as a top priority, for the diagnosis, management, and treatment of VS patients. The objectives of these guidelines are to establish the best evidence-based management of VSs, including initial otologic evaluation, imaging diagnosis, use of surgical techniques, assessment of tumor pathology, and the administration of radiation therapy. Because management of these tumors remains imperfect, it was also recommended that information on promising emerging therapies be assessed in the same manner to determine the possible application of these findings.
Having identified the topical objectives, the Guidelines Committee of the Joint Tumor Section recruited experts in the field from each of the parent organizations as lead writers of each section. These writers, in turn, recruited experts in non-neurosurgical specialties relevant to the field of management and therapy chosen. Writers were provided training on the CNS method of guideline development as used in this guideline set, using stepwise written instructions and then providing direct guidance as needed for each writer. The senior authors and CNS Guidelines Manager then assisted with the development of a step-by-step process to confirm that the methods were followed as the literature was collected and assessed and the documents developed. When writers were approached and preliminarily agreed to participate, they were asked to complete a formal conflict of interest questionnaire confirming the appropriateness of their participation. Writers also agreed to report any new conflicts of interest that might develop during the writing process. In this manner a multidisciplinary panel of writers referred to as the Vestibular Schwannoma Guidelines Task Force was assembled (Table 1), with significant administrative, logistical, and analytical support from the CNS Guidelines Committee. The method of this evidence-based clinical practice parameter has been written in a manner to be as transparent as possible using published assessment criteria.23,24
Topic Range of This Systematic Review and Evidence-Based Clinical Practice Guideline
Having identified writing groups for each topic, the members designed questions to allow assessment of the literature in a manner that would provide guidance for the management of VSs. These questions are presented at the beginning of each of the 9 guideline chapters spanning the topics of otologic assessment, imaging assessment, surgical resection, tumor evaluation by standard neuropathology and molecular techniques, radiation therapy, and emerging concepts and therapies. The questions developed for each section are summarized in Table 2.
Literature Examination Approach
A wide-ranging literature search strategy was undertaken to identify all citations relevant to the management of VSs. The PubMed and Embase electronic databases were searched from 1990 through 2014, with additional data being gleaned from the Cochrane Central Register of Controlled Trials and Web of Science. Other specialized databases considered are noted in the methods of the individual topic sections. The writing groups used the databases that provided the greatest breadth of nonoverlapping citations that were pertinent to answering the questions they had developed. Some databases may provide more information on therapy while others may provide more information on prognosis and diagnostic techniques, allowing the authors to make maximize the efficiency and value of their searches (Table 3). In addition, important articles from before this interval were reviewed and included if deemed to be critical evidence by the writing group. Such historic articles were subject to the same scrutiny for bias as manuscripts in the interval from 1990 through 2014 and those weaknesses pointed out when they were used. The search strategies used a combination of controlled vocabulary and text words. The specifics of the searches for a given topic are outlined in each respective guideline section. Reference lists of the publications chosen for full-text review were also screened for potentially relevant studies.
Study Selection, Quality Assessment, and Statistical Methods
The searches of the bibliographic databases identified possibly relevant citations for a given topic, and often these were large in number. The eligibility (inclusion/exclusion) criteria to screen the citations for each of the questions were determined ahead of time for each section by the respective writing group. These are documented in the individual clinical practice guideline sections in this series to assist the reader in understanding the development process. At least 2 authors evaluated the titles and abstracts using the inclusion and exclusion criteria with broad interpretation of the criteria being used initially, so as to maximize the likelihood of capturing pertinent information. Cases of disagreement about pertinence were resolved by a third author when needed. The full-text articles of the selected abstracts were then collected and the same process of applying the eligibility criteria was carried out again with the more in depth information available. Articles that met the eligibility criteria were grouped according to the questions they addressed and used to create the evidence tables and scientific foundation sections. Reasons for exclusion for papers were also documented to be able to discuss pertinent problem citations in the scientific foundation as needed.
Studies that met the eligibility criteria were subject to more detailed scrutiny and had their data extracted by 1 reviewer and the extracted information was checked by 1 or more other reviewers. Evidence and summary tables, reporting the extracted study information and evidence classification, were generated for all the included studies for each of the questions. Evidence tables were created with the most recent data first and subsequent listings in retrograde chronological order. The table headings consisted of first author name and year, followed by a brief study description, chosen data class, and conclusion. The authors were directed to craft the data in the tables in a succinct and fact-filled manner to allow for rapid understanding of the literature entry by the readership. The literature in the evidence tables was expanded upon in the Results section of each guideline article to emphasize important points supporting its classification and contribution to recommendations. The method by which this was accomplished is expanded upon in the Joint Guideline Committee (JGC) Guideline Development Methodology document. Internal drafts of the tables and manuscripts were developed by sharing them between writers electronically, by telephone, and in face-to-face meetings. Summary and conclusion statements were included for each section, with comments on key issues for future investigation being added where pertinent.
No question resulted in a collection of studies that warranted a meta-analysis.
AANS/CNS Evidence Classes and Levels of Recommendations
The evidence classifications were then used to create recommendations, the strength of which were graded according to the JGC Guideline Development Methodology (Tables 4–7). The class of evidence assigned to each study was based on study design (ie, class I, II, or III). The strength of the recommendations made (ie, level 1, 2, or 3) was directly linked to the evidence classification and took into account aspects of study quality and whether or not the plan was accomplished, not just study design. Specifically, the level of a recommendation made could be decreased, based on consensus input by the writing group, if there were methodological concerns regarding the studies that provided evidence for that particular recommendation.
Guideline Panel Consensus and Approval Process
As mentioned above, multidisciplinary writing groups were created for each section based on author expertise to address each of the disciplines and particular areas of therapy selected for these clinical guidelines. Each group was involved with literature selection, creation and editing of the evidence tables, and scientific foundations for their specific section and discipline. Using this information, the writing groups then drafted the recommendations in answer to the questions formulated at the beginning of the process, culminating in the clinical practice guideline for their respective discipline. The draft guidelines were then circulated to the entire clinical guideline panel to allow for multidisciplinary feedback, discussion, and ultimately approval.
The completed evidence-based clinical practice guidelines for the management of VSs were presented to the JGC of the AANS/CNS for review. The reviewers for the JGC were vetted by Neurosurgery for suitability and expertise to serve as reviewers for the purposes of publication in that journal also. The final product was then approved and endorsed by the executive committees of both the AANS and CNS before publication in Neurosurgery.
Development of this set of evidence-based clinical practice guidelines was editorially independent from the funding agencies. The funding agencies (the CNS Executive Committee and the AANS/CNS Joint Tumor Section Executive Committee) were permitted to review these guidelines only after the JGC had completed its extensive review, critique, and ultimate approval process. The funding groups then were limited to whether or not to endorse or reject this body of work, but substantive changes were not allowed. Figure 1 provides an outline of the key steps in the process of developing these clinical practice guidelines.
Summary
This series of guidelines was constructed to assess the most current and clinically relevant evidence for management of VSs to set a benchmark while also highlighting important key areas for future research. Only by designing future investigations in a high-quality manner that recognizes and overcomes previous weaknesses noted in these guidelines will advancement toward a remedy of this disease be achieved. Secondarily, the suggestions provided are set forth for conscientious use by the practicing physician who must consider all of the unique individual conditions in the therapy of a given person during his or her illness. The application of published guidelines information is an activity that results in strong and often polarized opinions. The guidelines presented in this current project are not meant to resolve these issues, and it is unlikely that any could accomplish such a goal. Fortunately, new research is constantly underway, and these guidelines are meant to be improved upon as this new evidence matures and is published. To that point, the data analyzed for this set of guidelines have been collected through 2014. This literature will be evaluated at least every 5 years and the guidelines will be reviewed and updated accordingly to ensure its continued validity and currency.
Conflict of Interest
The Vestibular Schwannoma Guidelines Task Force members reported all possible conflicts of interest (COIs) before beginning work on the guideline, using the COI disclosure form of the JGC, including potential COIs that are unrelated to the topic of the guideline. The CNS Guidelines Committee and Guideline Task Force Chair reviewed the disclosures and either approved or disapproved the nomination. The CNS Guidelines Committee and Guideline Task Force Chair are given latitude to approve nominations of Task Force Members with possible conflicts and address this by restricting the writing and reviewing privileges of that person to topics unrelated to the possible COIs (Table 8).
Acknowledgements
The guidelines task force would like to acknowledge the CNS Guidelines Committee for their contributions throughout the development of the guideline, the AANS/Congress of Neurological Surgeons Joint Guidelines Committee for their review, comments, and suggestions throughout peer review, as well as the contributions of Trish Rehring, MPH, CHES, Senior Manager of Clinical Practice Guidelines for the CNS, and Mary Bodach, MLIS, for assistance with the literature searches. Throughout the review process the reviewers and authors were blinded from one another. At this time the guidelines task force would like to acknowledge the following individual peer reviewers for their contributions: Sepideh Amin-Hanjani, MD, D. Ryan Ormond, MD, Andrew P. Carlson, MD, Kimon Bekelis, MD, Stacey Quintero Wolfe, MD, Chad W. Washington, MD, Cheerag Dipakkumar Upadhyaya, MD, and Mateo Ziu, MD.
Disclosures
These evidence-based clinical practice guidelines were funded exclusively by the CNS and the Section on Tumors of the Congress of Neurological Surgeons and the AANS, which received no funding from outside commercial sources to support the development of this document.
Table 1. Guideline Author
| Guideline Author |
Affiliations |
| Dare Adewumi, MD |
The Greater Houston Neurosurgery Center,
The Woodlands, Texas |
| Siviero Agazzi, MD, MBA |
Department of Neurosurgery and Brain Repair, College of Medicine,
University of South Florida,
Tampa, Florida |
| Anthony L. Asher, MD |
Carolina Neurosurgery & Spine Associates,
Charlotte, North Carolina |
| Tyler Atkins, MD |
Carolina Neurosurgery & Spine Associates,
Charlotte, North Carolina |
| Wenya Linda Bi, MD, PhD |
Department of Neurosurgery
Brigham and Women’s Hospital,
Harvard Medical School,
Boston, Massachusetts |
| Stuart H. Burri, MD |
Department of Radiation Oncology,
Levine Cancer Institute,
Charlotte, North Carolina |
| Matthew L. Carlson, MD |
Departments of Otorhinolaryngology and Neurosurgery,
Mayo Clinic School of Medicine,
Rochester, Minnesota |
| C. Eduardo Corrales, MD |
Division of Otolaryngology-Head and Neck Surgery,
Brigham and Women’s Hospital,
Harvard Medical School,
Boston, Massachusetts |
| Bradley Delman, MD |
Department of Radiology (Neuroradiology)
Icahn School of Medicine at Mount Sinai
New York, New York |
| Ian F. Dunn, MD |
Department of Neurosurgery
Brigham and Women’s Hospital,
Harvard Medical School,
Boston, Massachusetts |
| Kar-Ming Fung, MD, PhD |
Department of Pathology,
University of Oklahoma Health Sciences Center, Oklahoma City, Oklahoma |
|
Isabelle M. Germano, MD
|
Department of Neurosurgery,
Icahn School of Medicine at Mount Sinai,
New York, New York |
| Sheryl Green, MBBCh |
Department of Radiation Oncology,
Icahn School of Medicine at Mount Sinai,
New York, New York |
| Constantinos G. Hadjipanayis, MD, PhD |
Department of Neurosurgery,
Mount Sinai Beth Israel,
Icahn School of Medicine at Mount Sinai,
New York, New York |
| Steven N. Kalkanis, MD |
Department of Neurosurgery
Henry Ford Health System,
Detroit, Michigan |
| Michael J. Link, MD |
Department of Neurologic Surgery,
Mayo Clinic,
Rochester, Minnesota |
| D. Jay McCracken, MD |
Department of Neurosurgery,
Emory University School of Medicine,
Atlanta, Georgia |
| Srinivasan Mukundan, MD, PhD |
Division of Neuroradiology,
Brigham and Women’s Hospital,
Boston, Massachusetts |
| Brian A. Neff, MD |
Departments of Otorhinolaryngology and Neurosurgery,
Mayo Clinic, School of Medicine,
Rochester, Minnesota |
| Jeffrey J. Olson, MD |
Department of Neurosurgery,
Emory University School of Medicine,
Atlanta, Georgia |
|
Jonathan Parish, MD
|
Carolinas Medical Center,
Charlotte, North Carolina |
| Jo Elle G. Peterson, MD |
Department of Pathology,
University of Oklahoma Health Sciences Center, Oklahoma City, Oklahoma |
| Tarek A. Rayan, MD, PhD |
Department of Neurosurgery,
Mayo Clinic,
Rochester, MN |
| Timothy C. Ryken, MD |
Department of Neurosurgery,
Dartmouth University School of Medicine, Hanover, New Hampshire |
| Neil T. Shepard, MD, PhD |
Department of Otorhinolaryngology
Mayo Clinic, School of Medicine,
Rochester, Minnesota |
| Jason Sheehan, MD, PhD |
Department of Neurological Surgery,
University of Virginia,
Charlottesville, Virginia |
| Michael Sughrue, MD |
Department of Neurosurgery
University of Oklahoma,
Oklahoma City, Oklahoma |
| Alex D. Sweeney, MD |
Bobby R. Alford Department of Otolaryngology-Head and Neck Surgery,
Baylor College of Medicine,
Houston, Texas |
| Joon H. Uhm, MD |
Departments of Oncology and Neurology,
Mayo Clinic,
Rochester, Minnesota |
| Jamie J. Van Gompel, MD |
Departments of Otorhinolaryngology and Neurosurgery,
Mayo Clinic,
Rochester, Minnesota |
| Esther X. Vivas, MD |
Department of Otolaryngology-Head and Neck Surgery,
Emory University School of Medicine,
Atlanta, Georgia |
Table 2. Questions addressed in this guideline
| Guideline Topic |
Question |
|
Audiometric Methods in the Screening and Diagnosis of Vestibular Schwannomas
|
|
| |
What definition of asymmetric sensorineural hearing loss provides the optimal prognostic value for vestibular schwannoma diagnosis? |
| |
What is the significance of asymmetric tinnitus, defined as either purely unilateral or bilateral with subjective asymmetry, in the diagnosis of vestibular schwannomas? |
| |
What is the significance of sudden hearing loss with regard to vestibular schwannoma diagnosis? |
|
Hearing Preservation in Vestibular Schwannomas
|
|
|
Radiation
|
|
| |
What is the overall probability of maintaining serviceable hearing following single-fraction radiation therapy, utilizing modern dose planning, at two years, five years, and ten years following treatment? |
| |
Among patients with AAO-HNS class A or GR grade I hearing at baseline, what is the overall probability of maintaining serviceable hearing following single-fraction radiation therapy, utilizing modern dose planning, at two years, five years, and ten years following treatment? |
| |
What patient- and tumor-related factors influence progression to non-serviceable hearing following single-fraction stereotactic radiation treatment using < 14 Gy to the tumor margin? |
|
Surgery
|
|
| |
What is the overall probability of maintaining serviceable hearing following microsurgical resection of small to medium-sized sporadic vestibular schwannomas early after surgery, at two years, at five years, and at ten years following treatment? |
| |
Among patients with AAO-HNS class A or GR grade I hearing at baseline, what is the overall probability of maintaining serviceable hearing following microsurgical resection of small to medium-sized sporadic vestibular schwannomas early after surgery, at two years, at five years, and at ten years following treatment? |
| |
What patient- and tumor-related factors influence progression to non-serviceable hearing following microsurgical resection of small to medium-sized sporadic vestibular schwannomas? |
|
Observation
|
|
| |
What is the overall probability of maintaining serviceable hearing with conservative observation of vestibular schwannomas at two years, five years, and ten years following diagnosis? |
| |
Among patients with AAO-HNS class A or GR grade I hearing at baseline, what is the overall probability of maintaining serviceable hearing with conservative observation at 2 years, and 5 years following diagnosis? |
| |
What patient- and tumor-related factors influence progression to non-serviceable hearing during conservative observation? |
|
The Role of Imaging in the Diagnosis and Management of Vestibular Schwannomas
|
|
| |
What sequences should be obtained on MRI to evaluate vestibular schwannomas before and after surgery? |
| |
Is there a role for advanced imaging for facial nerve detection preoperatively (eg, CISS/FIESTA or DTI imaging)? |
| |
What is the expected growth rate of vestibular schwannomas on MRI, and how often should they be imaged if a “watch and wait” philosophy is pursued? |
| |
Do cystic vestibular schwannomas behave differently than their solid counterparts? |
| |
Should the extent of lateral internal auditory canal (IAC) involvement be considered by treating physicians? |
| |
How should patients with neurofibromatosis type 2 (NF2) and vestibular schwannoma be imaged and over what follow-up period? |
| |
How long should vestibular schwannomas be imaged after surgery, including after gross total, near total, and subtotal resection? |
|
The Role of Surgery in the Management of Vestibular Schwannomas
|
|
| |
What surgical approaches for vestibular schwannomas are best for complete resection and facial nerve (FN) preservation when serviceable hearing is present? |
| |
What surgical approaches for vestibular schwannomas are best for complete resection and FN preservation when serviceable hearing is not present? |
| |
Does vestibular schwannoma size matter for facial and vestibulocochlear nerve preservation with surgical resection? |
| |
Should small intracanalicular tumors be surgically resected? |
| |
Is hearing preservation routinely possible with vestibular schwannoma surgical resection? |
| |
When should surgical resection be the primary treatment in patients with NF2? |
| |
Does a multidisciplinary team, consisting of neurosurgery and neurotology, provide the best outcomes of complete resection and facial/vestibulocochlear nerve preservation for patients undergoing resection of vestibular schwannomas? |
| |
Does a subtotal surgical resection of a vestibular schwannoma followed by radiosurgery to the residual tumor provide comparable outcomes to patients who undergo a complete surgical resection? |
| |
Does surgical resection of vestibular schwannomas treat preoperative balance problems more effectively than stereotactic radiosurgery (SRS)? |
| |
Does surgical resection of vestibular schwannomas treat preoperative trigeminal neuralgia more effectively than SRS? |
| |
Is surgical resection of vestibular schwannomas more difficult (associated with higher facial neuropathies and subtotal resection rates) after initial treatment by SRS? |
|
Cranial Nerve Monitoring in Management of Vestibular Schwannomas
|
|
|
Facial Nerve
|
|
| |
Does intraoperative facial nerve monitoring during vestibular schwannoma surgery lead to better long-term facial nerve function? |
| |
Does intraoperative facial nerve monitoring allow the surgeon to accurately predict favorable long-term facial nerve function after vestibular schwannoma surgery? |
| |
Does an anatomically intact facial nerve with poor electromyogram electrical responses during intraoperative testing reliably predict poor long-term facial nerve function? |
|
Cochlear Nerve
|
|
| |
Is the use of intraoperative eighth cranial nerve monitoring associated with higher rates of hearing preservation following vestibular schwannoma resection? |
| |
Compared to far-field auditory brainstem response testing, is direct monitoring of the eighth cranial nerve associated with higher rates of hearing preservation following vestibular schwannoma resection? |
|
Pathology Techniques in the Diagnosis and Management of Vestibular Schwannomas
|
|
|
Pathology Techniques for Diagnosis
|
|
| |
What is the utility of frozen section diagnosis of vestibular schwannoma? |
| |
What is the utility of squash prep in vestibular schwannoma diagnosis? |
| |
What are the formal histopathologic features of VS on permanent sections? |
|
Pathology Techniques for Assessment of Prognosis
|
|
| |
What is the prognostic significance of Antoni A vs B histologic patterns in vestibular schwannomas? |
| |
What is the prognostic significance of mitotic figures seen in vestibular schwannoma specimens? |
| |
Are there other light microscopic features that predict clinical behavior of vestibular schwannomas? |
| |
Does the KI-67 labeling index predict clinical behavior of vestibular schwannomas? |
| |
Does the proliferating cell nuclear antigen labeling index predict clinical behavior of vestibular schwannomas? |
| |
Does degree of vascular endothelial growth factor expression predict clinical behavior of vestibular schwannomas? |
|
The Role of Radiation Therapy in the Management of Vestibular Schwannomas
|
|
| |
What are the indications for radiosurgery (SRS) treatment versus observation for patients with intracanalicular vestibular schwannomas without evidence of radiographic progression? |
| |
Is there a difference in outcome based on radiosurgery equipment used: Gamma Knife versus LINAC-based radiosurgery versus proton beam? |
| |
Is there a difference in outcome based on the dose delivered? |
| |
Is there a difference in outcome based on the number of fractions? |
| |
What is the best time sequence for follow-up images after SRS? |
| |
Is there a role for retreatment? |
| |
What is the risk of radiation-induced malignant transformation of vestibular schwannomas treated with SRS? |
| |
What are the indications for SRS in patients with neurofibromatosis type 2? |
|
Emerging Modalities in the Diagnosis and Management of Vestibular Schwannomas
|
|
|
Medical Therapies
|
|
| |
What is the role of bevacizumab in the treatment of patients with vestibular schwannomas? |
| |
What is the role of AR42, a histone deacetylase inhibitor, in the treatment of patients with vestibular schwannomas? |
| |
Is there a role for imatinib mesylate, lapatinib, erlotinib, or everolimus in the treatment of patients with vestibular schwannomas? |
| |
What is the role of aspirin, to augment inflammatory response, in the treatment of patients with vestibular schwannomas? |
| |
Is there a role for treatment of vasospasm, ie, nimodipine or hydroxyethyl starch, perioperatively to improve facial nerve outcomes in patients with vestibular schwannomas? |
|
Prehabilitation
|
|
| |
Is there a role for preoperative vestibular rehab or vestibular ablation with gentamicin for patients surgically treated for vestibular schwannomas? |
|
Surgery
|
|
| |
Does endoscopic assistance make a difference in resection or outcomes in patients with vestibular schwannomas? |
|
Pathology
|
|
| |
Are there molecular or histologic markers that can predict response to or guide targeted medical therapies of vestibular schwannomas? |
AAO-HNS, American Academy of Otolaryngology-Head and Neck Surgery; CISS, constructive interference steady state; DTI, diffusion tensor imaging; FIESTA, fast imaging employing steady-state acquisition; FN, facial nerve; GR, Gardner–Robertson hearing classification; IAC, internal auditory canal; LINAC, linear accelerator; MRI, magnetic resonance imaging; NF2, neurofibromatosis type 2; SRS, stereotactic radiosurgery; VS, vestibular schwannoma.
Table 3. Databases searched by section
| Section |
Database Searched |
| Audiologic screening |
PubMed, Embase, Web of Science |
| Hearing preservation outcomes |
PubMed, Embase, Web of Science |
| Cranial nerve monitoring |
PubMed, Embase, Web of Science |
| Imaging |
PubMed, Cochrane Central |
| Surgical resection |
PubMed, Cochrane Central |
| Pathology methods and prognostic factors |
PubMed, Cochrane Central |
| Radiosurgery and radiation therapy |
PubMed, Cochrane Central |
| Emerging therapies |
PubMed, Cochrane Central |
Table 4. American Association of Neurological Surgeons/Congress of Neurological Surgeons classification of evidence on therapeutic effectiveness and levels of recommendation
| Evidence Classification |
|
Class I
|
Evidence provided by one or more well-designed randomized controlled clinical trials, including overview (meta-analyses) of such trials |
| Class II |
Evidence provided by well-designed observational studies with concurrent controls (eg, case-control and cohort studies) |
| Class III |
Evidence provided by expert opinion, case series, case reports, and studies with historical controls |
| Levels of Recommendation |
| Level 1 |
Generally accepted principles for patient management, which reflect a high degree of clinical certainty (usually this requires class I evidence which directly addresses the clinical questions or overwhelming class II evidence when circumstances preclude randomized clinical trials) |
| Level 2 |
Recommendations for patient management which reflect clinical certainty (usually this requires class II evidence or a strong consensus of class III evidence) |
| Level 3 |
Other strategies for patient management for which the clinical utility is uncertain (inconclusive or conflicting evidence or opinion) |
Table 5. American Association of Neurological Surgeons/Congress of Neurological Surgeons classification of evidence on diagnosis and levels of recommendation
|
Class I evidence
Level 1 recommendation |
Evidence provided by one or more well-designed clinical studies of a diverse population using a “gold standard” reference test in a blinded evaluation appropriate for the diagnostic applications and enabling the assessment of sensitivity, specificity, positive and negative predictive values, and, where applicable, likelihood ratios. |
|
Class II evidence
Level 2 recommendation |
Evidence provided by one or more well-designed clinical studies of a restricted population using a “gold standard” reference test in a blinded evaluation appropriate for the diagnostic applications and enabling the assessment of sensitivity, specificity, positive and negative predictive values, and, where applicable, likelihood ratios. |
|
Class III evidence
Level 3 recommendation |
Evidence provided by expert opinion or studies that do not meet the criteria for the delineation of sensitivity, specificity, positive and negative predictive values, and, where applicable, likelihood ratios. |
Table 6. American Association of Neurological Surgeons/Congress of Neurological Surgeons classification of evidence on clinical assessment and levels of recommendation
|
Class I evidence
Level 1 recommendation |
Evidence provided by one or more well-designed clinical studies in which interobserver and/or intraobserver reliability is represented by a kappa statistic ≥0.60. |
|
Class II evidence
Level 2 recommendation |
Evidence provided by one or more well-designed clinical studies in which interobserver and/or intraobserver reliability is represented by a kappa statistic ≥0.40. |
|
Class III evidence
Level 3 recommendation |
Evidence provided by one or more well-designed clinical studies in which interobserver and/or intraobserver reliability is represented by a kappa statistic <0.40. |
Table 7. American Association of Neurological Surgeons/Congress of Neurological Surgeons classification of evidence on prognosis and levels of recommendation
To evaluate papers addressing prognosis, 5 technical criteria are applied:
- Was a well-defined representative sample of patients assembled at a common (usually early) point in the course of their disease?
- Was patient follow-up sufficiently long and complete?
- Were objective outcome criteria applied in a “blinded” fashion?
- If subgroups with different prognoses were identified, was there adjustment for important prognostic factors?
- If specific prognostic factors were identified, was there validation in an independent “test set” group of patients?
|
Class I evidence
Level 1 recommendation |
All 5 technical criteria above are satisfied |
|
Class II evidence
Level 2 recommendation |
Four of 5 technical criteria are satisfied |
|
Class III evidence
Level 3 recommendation |
Everything else |
Table 8. Conflict of interest disclosures
| Guideline Author |
Potential Conflict(s) of Interest |
| Anthony L. Asher, MD |
- HyperBranch: Stock Shareholder
|
| Stuart H. Burri, MD |
- Novocure: Honorarium
|
| Isabelle M. Germano, MD |
- Brainlab: Consultant Fee
- ElMindA: Stock Shareholder
- Surgical Theater: Stock Shareholder
- Lazarus: Stock Shareholder
- NYU Stern School of Business: Other Financial Support
|
| Constantinos G. Hadjipanayis, MD, PhD |
- NIH/NCI: Grants/Research Support
- NX Development Corp: Grants/Research Support
- NX Development Corp: Consultant Fee
- Meditech, LLC: Consultant Fee
|
| Jeffrey J. Olson, MD |
- American Cancer Society: Consultant Fee
|
| Timothy C. Ryken, MD |
- Medtronic, Inc: Consultant Fee
- EBM Care, Inc: Consultant Fee
- K2M Spine, Inc: Honorarium
- Arbor Pharmaceuticals: Honorarium
|
| Alex D. Sweeney, MD |
- Advanced Bionics Corp: Consultant Fee
- Med-El Gmbh (2015), Cochlear Corp (2016): Travel Support to Research Meetings
|
| Jamie J. Van Gompel, MD |
- Federal Co-Investigator: Neurophysiologically based brain state tracking and modulation in focal epilepsy funded by NIH (UH2 NS95495) 09/2015-07/2018: Grants/Research Support
- Storz: Education Grant
- NeuroOne: Stockholder
|
NCI, National Cancer Institute; NIH, National Institutes of Health.
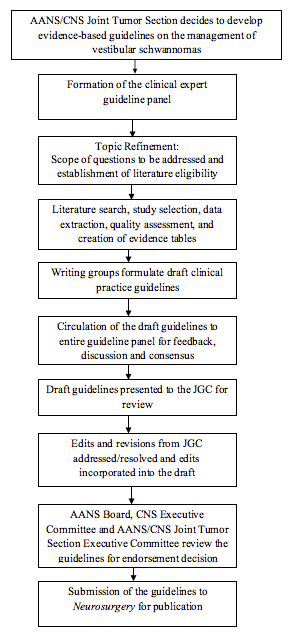
Figure 1. An outline of the key steps in the process of developing these clinical practice guidelines. AANS, American Association of Neurological Surgeons; CNS, Congress of Neurological Surgeons; JGC, Joint Guidelines Committee.
References
- Kshettry VR, Hsieh JK, Ostrom QT, Kruchko C, Barnholtz-Sloan JS. Incidence of vestibular schwannomas in the United States. J Neurooncol 2015;124(2):223-228.
- Evans DG, Howard E, Giblin C, et al. Birth incidence and prevalence of tumor-prone syndromes: estimates from a UK family genetic register service. Am J Med Genet A 2010;152a(2):327-332.
- Cooper J, Giancotti FG. Molecular insights into NF2/Merlin tumor suppressor function. FEBS Lett 2014;588(16):2743-2752.
- Aarhus M, Bruland O, Saetran HA, Mork SJ, Lund-Johansen M, Knappskog PM. Global gene expression profiling and tissue microarray reveal novel candidate genes and down-regulation of the tumor suppressor gene CAV1 in sporadic vestibular schwannomas. Neurosurgery 2010;67(4):998-1019.
- Sughrue ME, Yeung AH, Rutkowski MJ, Cheung SW, Parsa AT. Molecular biology of familial and sporadic vestibular schwannomas: implications for novel therapeutics. J Neurosurg 2011;114(2):359-366.
- Carlson ML, Tveiten OV, Driscoll CL, et al. Long-term quality of life in patients with vestibular schwannoma: an international multicenter cross-sectional study comparing microsurgery, stereotactic radiosurgery, observation, and nontumor controls. J Neurosurg 2015;122(4):833-842.
- Ramsden RT. ‘A brilliant surgical result, the first recorded’: Annandale’s case, 3 May 1895. J Laryngol Otol May 1995;109(5):369-373.
- Cushing H. Tumors of the Nervus Acusticus and the Syndrome of the Cerebellopontile Angle. Philadelphia (PA): W. B. Saunders; 1917.
- Cushing H. Further concerning the acoustic neuromas. Laryngoscope 1921;31(4):209-228.
- Dandy W. An operation for the total extirpation of tumors of the cerebellopontine angle. A preliminary report. Bull Johns Hopkins Hosp 1922;33:344-345.
- Dandy W. An operation for the total removal of cerebellopontine (acoustic) tumors. Surg Gynecol Obstet 1925;41:129-148.
- Dandy W. Removal of cerebellopontile (acoustic) tumors by the unilateral approach. Arch Surg 1934;29(3):337-344.
- Dandy W. Results of removal of acoustic tumors by the unilateral approach. Arch Surg 1941;42(6):1026-1033.
- Parry D. A case of tinnitus treated by division of the auditory nerve. J Laryngol Otol 1904;19:402-406.
- Quix F. Ein fall von translabyrintharisch operiertem tumor acousticus. Verh Dtsch Otol Ges 1912;21:244-255.
- House WF. Transtemporal bone microsurgical removal of acoustic neuromas. Report of cases. Arch Otolaryngol 1964;80:617-667.
- Leksell L. The stereotaxic method and radiosurgery of the brain. Acta Chir Scand 1951;102(4):316-319.
- Leksell L. A note on the treatment of acoustic tumours. Acta Chir Scand 1971;137(8):763-765.
- Mautner VF, Nguyen R, Kutta H, et al. Bevacizumab induces regression of vestibular schwannomas in patients with neurofibromatosis type 2. Neurooncol 2010;12(1):14-18.
- Kano H, Kondziolka D, Khan A, Flickinger JC, Lunsford LD. Predictors of hearing preservation after stereotactic radiosurgery for acoustic neuroma. J Neurosurg 2009;111(4):863-873.
- Tamura M, Carron R, Yomo S, et al. Hearing preservation after gamma knife radiosurgery for vestibular schwannomas presenting with high-level hearing. Neurosurgery 2009;64(2):289-296.
- Turel MK, Thakar S, Rajshekhar V. Quality of life following surgery for large and giant vestibular schwannomas: a prospective study. J Neurosurg 2015;122(2):303-311.
- Reames BN, Krell RW, Ponto SN, Wong SL. Critical evaluation of oncology clinical practice guidelines. J Clin Oncol 2013;31(20):2563-2568.
- Institute of Medicine Committee on Standards for Developing Trustworthy Clinical Practice Guidelines. Clinical Practice Guidelines We Can Trust. Washington (DC): National Academies Press; 2011.
© Congress of Neurological Surgeons
Source: Neurosurgery, February 2018