Guidelines for the Treatment of Adults with Metastatic Brain Tumors
8. The Role of Prophylactic Anticonvulsants in the Treatment of Adults with Metastatic Brain Tumors
Download PDF Neurosurgery, 2019
Sponsored by: The Congress of Neurological Surgeons and the Section on Tumors
Affirmation of Educational Benefit by: The Congress of Neurological Surgeons and the American Association of Neurological Surgeons
Clark C. Chen, MD, PhD1, Robert C. Rennert, MD2, Jeffrey J. Olson, MD3
- Department of Neurosurgery, University of Minnesota Medical School, Minneapolis, Minnesota, USA
- Department of Neurosurgery, University of California, San Diego, LaJolla, California, USA
- Department of Neurosurgery, Emory University School of Medicine, Atlanta, Georgia, USA
Correspondence:
Clark C. Chen, MD, PhD
Lyle A. French Chair in Neurosurgery
Professor and Department Head of Neurosurgery
University of Minnesota Medical School
D429 Mayo Memorial Building
420 Delaware Street S.E., MMC 96
Minneapolis, MN 55455
E-mail: ccchen@umn.edu
Tel: 612-626-5767
Fax: 612-624-0644
Disclaimer of Liability
This clinical systematic review and evidence-based guideline was developed by a multidisciplinary physician volunteer task force and serves as an educational tool designed to provide an accurate review of the subject matter covered. These guidelines are disseminated with the understanding that the recommendations by the authors and consultants who have collaborated in their development are not meant to replace the individualized care and treatment advice from a patient's physician(s). If medical advice or assistance is required, the services of a competent physician should be sought. The proposals contained in these guidelines may not be suitable for use in all circumstances. The choice to implement any particular recommendation contained in these guidelines must be made by a managing physician in light of the situation in each particular patient and on the basis of existing resources.
Keywords:
Brain metastases, cerebral metastases, anti-epileptic drugs, seizure, craniotomy
Abbreviations
AED: Anti-epileptic drug
HGG: High-grade glioma
PHT: Phenytoin
ABSTRACT
Target Populations: Adults with solid brain metastases who have not experienced a seizure.
Question 1: Do prophylactic anti-epileptic drugs (AEDs) decrease the risk of seizures in non-surgical patients with brain metastases who are otherwise seizure free?
Recommendation:
Level 3: Prophylactic AEDs are not recommended for patients with brain metastases who did not undergo surgical resection and are otherwise seizure-free.
Question 2: Do prophylactic AEDs decrease the risk of seizures in patients with brain metastases and no prior history of seizures in the postoperative setting?
Recommendation:
Level 3: Routine post-craniotomy anti-epileptic drug use for seizure-free patients with brain metastases is not recommended.
INTRODUCTION
Rationale
Brain metastases occur in <30% of patients with systemic cancers. 1 Seizures are a common sequela of brain metastases due to disruption of neurotransmitters by cancer cells, general cerebral edema, or local mass effect.2, 3 Anti-epileptic drug (AED) use after seizure occurrence is well-established in patients with brain metastases. 3 However, the efficacy of prophylactic AEDs for patients with brain metastases who do not undergo surgery remains an unresolved issue.
Another issue in the management of patients with brain metastases involves whether prophylactic AED use is warranted in the postoperative setting for patients without a prior history of seizures. Surgical resection is frequently performed for symptomatic brain metastases.4 Surgical manipulation of the cerebrum has also been associated with increase seizure risk.5 In this context, it remains unclear whether prophylactic AED use is appropriate in the postoperative setting for patients with brain metastases who are otherwise seizure-free. Previous guidelines from 2010 do not recommend prophylactic AED use for patients with brain metastases without a seizure history. These guidelines are based on a single study of largely non-surgical patients.6
Objectives
The objective of this guideline is to address the role of AED prophylaxis in patients with brain metastases without prior seizures in the 1) non-surgical and 2) postoperative settings.
METHODS
Writing group and question establishment
The Joint Tumor Section of the American Association of Neurological Surgeons (AANS) and the Congress of Neurological Surgeons (CNS) identified an update of the metastatic brain tumor guidelines as a topic worthy of guideline development. Members of the Tumor Section, as well as other neurosurgeons and members of other specialties commonly involved in the management of metastatic brain tumors were identified to form the Metastatic Brain Tumor Evidence-Based Practice Guideline Task Force (ie, the “task force”). The writers were then divided up into topic sections and developed pertinent questions for those topics. These were circulated among the entire task force, modified, and agreed upon. With these questions in hand, the literature searches, such as the one described below, were executed. Additional details regarding the literature search and review methodology can be found in the introductory section of this set of guidelines. This guideline was then developed using multiple iterations of written review conducted by the authors, then by members of the task force, and finally by AANS/CNS Joint Guidelines Review Committee (JGRC).
Search strategy
The PubMed online database was searched from January 1, 1990, through December 31, 2015, using the following query: (craniotomy OR postcraniotomy OR post-craniotomy OR brain metastasis OR brain metastases OR central nervous system metastasis OR central nervous system metastases OR metastatic brain cancer OR brain mets OR metastatic cancer brain OR secondary brain neoplasm OR brain neoplasm OR brain tumor OR brain tumour OR cerebral tumor OR cerebral tumour OR cerebral metastasis OR cerebral metastases) AND (anticonvulsant OR seizure OR seizures OR antiepileptic drug OR anti-epileptic drug OR antiepileptic OR anti-epileptic OR anti-convulsant OR AED OR seizure prophylaxis). This inclusive search strategy was designed to capture all manuscripts pertaining to brain metastases and seizures for manual review.
Study selection and eligibility criteria
The following inclusion criteria were used for manual review of studies:
1. Published in English with a publication date of January 1, 1990, through December 31, 2015.
2. Included patients with brain metastases.
3. Published in a peer-reviewed journal with comparative data pertaining to seizure risk including patients with brain metastases (study designs for primary data collection included randomized controlled trials, non-randomized trials, cohort studies, case–control studies, and observational or retrospective studies).
4. Number of study subjects with brain metastases ≥10.
5. Provided information regarding use of AEDs and the relationship of seizures to surgical intervention for study participants with brain metastases.
6. Provided a comparison cohort to brain metastases patients without prophylactic AED treatment.
Studies reporting data solely on stereotactic radiosurgery or experimental drug therapies for metastases were excluded. Two reviewers evaluated search-returned citations via an initial title/abstract screen for relevance based on the above pre-determined criteria.
Data collection process
A secondary full-text review of potentially relevant manuscripts was conducted by two reviewers with detailed attention to the above inclusion/exclusion criteria. Data from studies meeting eligibility criteria were data extracted by a single reviewer and checked by a second reviewer.
Assessment for risk of bias
Included studies were assessed for potential bias upon full-text review by two reviewers. Specific areas of bias assessed for included selective data reporting/analysis regarding metastases subgroups, loss of data points over time, ascertainment bias, early termination/power biases, and retrospective data/causation bias.
Evidence classification and recommendation levels
The quality of each study regarding metastases-specific data and the strength of the recommendations within this work were graded according to the American Association of Neurological Surgeons (AANS)/Congress of Neurological Surgeons (CNS) criteria (here.). In brief, Class I evidence is from well-designed randomized controlled clinical trials, Class II evidence is from case-control and cohort studies, and Class III evidence is provided by expert opinion, case series, or studies with historical controls. Level 1 recommendations reflect a high degree of clinical certainty generally based on Class I data, Level 2 recommendations reflect clinical certainty based generally on Class II data, and Level 3 recommendations reflect clinical uncertainty based on inconclusive or conflicting evidence.
RESULTS
Study selection and characteristics
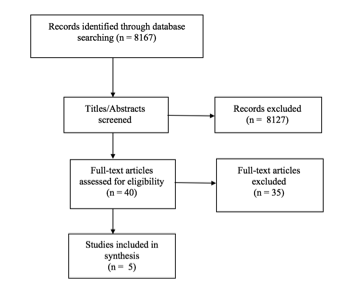
The literature search yielded 8167 studies that met the above criteria, of which, 8127 studies were excluded during title/abstract review. The remaining 40 studies underwent full-text review, and 35 studies were excluded due to limited metastases-specific data, a lack of information regarding use of AEDs, lack of information on surgical intervention, lack of a comparison cohort without AED prophylaxis, or other predefined exclusion criteria. Five studies met all inclusion criteria (Figure 1).
Results of individual studies, discussion of study limitations and risk of bias
Seizure prophylaxis in patients with brain metastases who did not undergo surgery
Two studies met inclusion criteria and provided information pertaining to the use of prophylactic AEDs in patients with brain metastases 1) who did not have prior histories of seizure and 2) the majority of whom did not undergo surgery (Table 1).
Forsyth et al7 randomized 100 brain tumor patients with no prior history of seizure to receive either 1) AED for 3 months, in the form of phenytoin (PHT) or phenobarbital, or 2) no AED. Sixty of the 100 (60%) patients suffered from brain metastases (92% of the remaining 40 patients suffered from high-grade glioma [HGG]). Fifty-two of the brain metastases patients (87%) did not undergo surgical intervention of any form. The primary study endpoint was seizure occurrence (<3 months), and a secondary endpoint was adverse drug reactions. Baseline characteristics of the 2 arms were generally comparable. The overall study showed that seizures occurred in 26% of patients treated with AEDs and 15% in the non-AED group (p= .98). Minor adverse events (nausea and rash) occurred in 7 AED-treated patients (16%), and major adverse events (myelosuppression and ataxia) occurred in 3 AED-treated patients (6%). Of the patients with brain metastases, 26 were treated with AEDs and 34 were not. Notably, ~30% of patients with brain metastases died prior to the 3-month follow-up. Within the brain metastases subgroup, there was no significant difference in 3-month seizure rates between groups (10% vs 13%, p = .90). Notably, the same results were observed for patients with HGG. The trial was terminated early based on the observed seizure frequency of ~10%, suggesting a high probability of data insufficiency for the primary endpoint. The data pertaining to metastases in this study were deemed to be Class III due to early study termination and a power bias to identify only large reductions in seizure rates.
Glantz et al8 randomized 74 brain tumor patients with no prior history of seizures to receive either 1) valproate (VAL), or 2) placebo for the duration of the study. Fifty-nine of these patients (80%) suffered from brain metastases (9 of 74 patients [12%] were diagnosed with glioblastoma). Sixty-six percent of the randomized patients did not undergo surgery of any form. The primary study endpoints were new onset seizure or death within 12 months of enrollment. Baseline characteristics of the 2 arms were generally comparable. The overall study showed that seizures occurred in 35% of patients treated with VAL and 24% in the placebo group (p = .3). By the end of the study, 26 of 37 (70%) VAL-treated patients had died, and 27 of 37 (73%) placebo-treated patients died. Insufficient data were included in the published article to allow post-hoc analysis specific to the 77% of the patients who suffered from brain metastases. The data pertaining to metastases in this study were deemed to be Class III due to a lack of subgroup analysis bias for this population.
Synthesis of results
Of the 2 studies identified pertaining to the use of prophylactic AEDs in patients with brain metastases, neither found a beneficial effect of AEDs on seizure rates. However, 1 study was terminated early because the proposed sample size was underpowered to detect lowered seizure risk attributable to AEDs, and the other study enrolled a similar number of patients but did not provide metastases-specific analysis. These studies are Class III evidence,9 leading to the Level 3 recommendation that the use of prophylactic AEDs is not justified for patients with brain metastases who did not undergo surgical resection and are otherwise seizure-free.
Results of individual studies, discussion of study limitations and risk of bias
Seizure prophylaxis in patients with brain metastases in the postoperative setting
Three studies met the inclusion criteria and provided information pertaining to the use of post-craniotomy prophylactic AEDs in brain tumor patients without preoperative seizures (Table 2).
Ansari et al10 retrospectively reviewed AED use and seizure frequency in 202 patients with no previous seizure history who underwent craniotomies for intra-axial brain tumors. Eighty-six of the 202 patients (43%) in this study suffered from brain metastases (36% of 202 patients suffered from glioblastoma). The overall study showed that 22.8 % of patients had postoperative seizures (median follow-up 321 days). No significant difference was found in patients who received prophylactic AEDs administered based on surgeon preference when compared with patients who were not taking prophylactic AEDs (p = .2867). Nineteen percent of patients with metastases experienced seizures. Insufficient data were provided to complete a post-hoc metastases specific analysis. The metastases data in this study were deemed to be Class III due a selective case/data reporting bias from a lack of subgroup analysis for this patient population.
Wu et al.,11 randomized 123 brain tumor patients with no prior seizure history to PHT or no AED in the postoperative setting for a 7-day duration. Seventy-seven of 123 patients (62%) in this study suffered from brain metastases (80% of the remaining 46 patients suffered from HGG). The primary study endpoint was seizure occurrence (<30 days), and a secondary endpoint was the occurrence of adverse reactions to phenytoin. Baseline characteristics of the 2 arms were generally comparable. The overall study results showed that 24% of the PHT group suffered seizures within 30 days of surgery while 18% of the no AED cohort suffered seizure within 30 days (p = .51). Significantly more adverse events were noted with PHT versus no AEDs (14% [n = 18] vs 0%, p = .01). Of the patients with brain metastases, 5% and 3% suffered seizures within 30 days in the no AED and PHT groups, respectively (p = .62). Thirteen percent and 8% suffered seizures that occurred after 30 days in the no AED and PHT groups, respectively (p =.71). Seizure onset within 30 days of surgery was not associated with seizure after 30 days. Seven PHT-treated metastases patients (9%) suffered adverse events. Similar results were observed for the HGG patients. The trial was terminated early based on an independent interim data analysis suggesting that a significantly larger sample size would be required to adequately address the hypothesis. The data pertaining to metastases in this study were deemed to be Class III due to early study termination and a power bias to identify only large reductions in seizure rates.
Franceschetti et al12 randomized 63 brain tumor patients without prior history of seizures to AEDs (phenobarbital or PHT, n = 41) or no AED (n = 22) in the postoperative setting. Anti-epileptic drugs were maintained for the duration of the study. Thirteen of 63 (21%) patients in this study suffered from brain metastases (23 of 63 patients [37%] suffered from HGG; 27 of 63 patients [42%] were afflicted with meningiomas). The end points assessed were early (<1 week) and late (>1 week) postoperative seizures. Baseline characteristics of the 2 arms were generally comparable. The overall study results showed that early postoperative seizures occurred in 7% of the AED cohort and 18% of the non-AED cohort (p = .23). Late postoperative seizures occurred in 12% of the AED cohort and 21% of the non-AED cohort (p = .64). Seizure <1 week was not associated with seizure >1 week. Overall, the study found increased risk of seizure without prophylactic AED. However, this risk was not statistically significant. Insufficient data were included in the published article to allow post-hoc analysis specific to the 21% of the patients who suffered from brain metastases. Data pertaining to metastases from this study were deemed to be Class III due to a lack of subgroup analysis bias for this population.
Synthesis of results
Of the 3 studies identified analyzing the use of prophylactic AEDs in patients with brain metastases in the postoperative setting, none found a beneficial effect of AEDs on postoperative seizure rates. One study was nonetheless terminated early when the proposed sample size was found to be underpowered for detection of lowered seizure risk from AEDs. The remaining 2 studies enrolled/reviewed a similar number of patients as the terminated study, but did not provide metastases-specific analyses. These works are Class III evidence,9 leading to the Level 3 recommendation that routine use of prophylactic postoperative AEDs is not justified for patients with brain metastases who are otherwise seizure-free.
DISCUSSION
While the studies do not conclusively resolve the issue of AED use in seizure-free patients with brain metastases, they do provide estimates of the seizure risk in this population. The risk of seizure in these cohorts who largely did not undergo surgical intervention ranged from 26% to 35%. 7, 8 The 3 studies of post-craniotomy patients with brain metastases also provide estimates of seizure risk in this setting. In the immediate postoperative period, the risk of seizure is ~5% within the first 30 days and 8% to 13% after the first 30 days. Early seizure onset (< 30 days) is not associated with an increased risk of late onset seizure (>30 days). The cumulative seizure risk for patients with brain metastases in the postoperative setting (<30 plus >30 days) is remarkably similar to those reported in the non-surgical patients, suggesting that surgical resection does not significantly increase the risk of seizure. In the 2 studies with data sufficiently granular as to allow for comparison of brain metastasis and HGG,7, 11 the seizure risk in these patient populations appears similar.
The authors’ interpretation of the available data is that if AEDs reduce seizure risk in seizure-free patients with brain metastases in the non-surgical or surgical setting, the effect is unlikely to be a dramatic one. As such, the task force cautions against chronic AED prophylaxis in these populations, particularly given that adverse effects are reported in 10% to 22% of the cohorts with chronic AED use. Insufficient data were presented in the article to allow metastases-specific sub-group analysis in a post-hoc manner. In this context, the task force cautions against routine AED prophylaxis for patients in the non-surgical or surgical setting with brain metastases, who are otherwise seizure-free (Level 3 recommendations).
CONCLUSION AND KEY ISSUES FOR FUTURE INVESTIGATIONS
Fundamentally, future studies of prophylactic AED use in patients with brain metastases can take on 1 of 2 forms. The first involves a cost-benefit analysis to define the level of efficacy that society, in general, is willing to accept for prophylactic AEDs and designing a study of appropriate sample size. For instance, cholesterol-lowering statins are commonly accepted as an efficacious medication for patients with elevated cardiac risk. Meta-analysis of the “overall net benefit” of statins suggest that treatment of patients with low cardiac risk with statins for 5 years will lower mortality risk by ~10%.13 If this 10% threshold is imposed as the acceptable efficacy threshold for prophylactic AEDs in the seizure-free brain metastasis population, then ~6200 patients would need to be enrolled to achieve a sample size sufficient to detect this effect size (assuming 20% of brain metastasis patients suffer seizures, an a of 0.05 (2-tailed) and a b of 0.8). Such a study would likely require a collaborative consortium. Alternatively, studies can be carried out to define “high-risk” brain metastasis patients who are more likely to suffer from seizures from brain metastasis (eg, brain metastases in epileptic areas of the cerebrum or with genomic profiles associated with epileptogenic processes).2 A randomized controlled trial with the appropriate sample size can then be designed to test the efficacy of prophylactic AEDs in these patient populations. Additional considerations in future studies on the topic include the dedicated study of AEDs for brain metastases (apart from gliomas), or a breakdown of data by tumor type in heterogeneous studies to allow for secondary metastases-specific analyses.
The available data do not suggest that routine AED use significantly reduces seizure risk in patients with brain metastases who were previously seizure-free. However, published studies suggest that seizure risk may be elevated after surgical manipulation of seizure-prone cerebrum. 5, 14 Moreover, the risk of adverse events related to a short course of AEDs is exceedingly low. In 1 study, the only adverse event attributable to a 7-day course of levetiracetam in the post-craniotomy setting was modest levels of somnolence in ~4% of treated patients; somnolence uniformly resolved after discontinuation of the AED. 15 Further studies with focus on these newer AED in BM patients deemed at risk for seizure should be considered. Until these studies are completed, prophylactic AED use in patients with brain metastases will remain more art than science.
Potential Conflicts of Interest
The Brain Metastases Guideline Update Task Force members were required to report all possible conflicts of interest (COIs) prior to beginning work on the guideline, using the COI disclosure form of the AANS/CNS Joint Guidelines Review Committee, including potential COIs that are unrelated to the topic of the guideline. The CNS Guidelines Committee and Guideline Task Force Chair reviewed the disclosures and either approved or disapproved the nomination. The CNS Guidelines Committee and Guideline Task Force Chair are given latitude to approve nominations of task force members with possible conflicts and address this by restricting the writing and reviewing privileges of that person to topics unrelated to the possible COIs. The conflict of interest findings are provided in detail in the companion introduction and methods manuscript (here).
Disclosures
These evidence-based clinical practice guidelines were funded exclusively by the Congress of Neurological Surgeons and the Tumor Section of the Congress of Neurological Surgeons and the American Association of Neurological Surgeons, which received no funding from outside commercial sources to support the development of this document.
ACKNOWLEDGEMENTS
The authors acknowledge the CNS Guidelines Committee for its contributions throughout the development of the guideline and the AANS/CNS Joint Guidelines Review Committee for its review, comments, and suggestions throughout peer review, as well as Trish Rehring, MPH, CHES, CNS Guidelines Senior Manager, and Mary Bodach, MLIS, Senior Guidelines Specialist, for their assistance. Throughout the review process, the reviewers and authors were blinded from one another. At this time, the guidelines task force would like to acknowledge the following individual peer reviewers for their contributions: Manish Aghi, MD, PhD, Manmeet Ahuwalia, MD, Sepideh Amin-Hanjani, MD, Edward Avila, MD, Maya Babu, MD, MBA, Kimon Bekelis, MD, Priscilla Brastianos, MD, Paul Brown, MD, Andrew Carlson, MD, MS, Justin Jordan, MD, Terrence Julien, MD, Cathy Mazzola, MD, Adair Prall, MD, Shayna Rich, MD, PhD, Arjun Sahgal, MD, Erik Sulman, MD, May Tsao, MD, Michael Voglebaum, MD, Stephanie Weiss, MD, and Mateo Ziu, MD.
Figure 1. PRISMA diagram showing flow of study evaluation for inclusion
id="chapter8Table1"Table 1. Summary of published data on prophylactic seizure medication in patients with brain metastases
|
Author (Year)
|
Description of Study
|
Data Class
|
Conclusions
|
|
Forsyth et al,7 2003
|
Multi-institutional, prospective, randomized controlled trial of PHT or phenobarbital vs no seizure prophylaxis (control) in patients with newly diagnosed cerebral metastases.
Patients with systemic cancer (breast, lung, melanoma, and other) with typical radiographic appearance of brain metastases, recruited within 1 month of diagnosis, and no prior seizures.
A total of 100 study patients enrolled, 52 with metastases (23 AED group, 29 no AED control); 8 additional patients randomized after diagnosis via craniotomy or biopsy.
|
III
|
Trial terminated early based on a high probability of data insufficiency. No significant difference in 3-month seizure rates between groups (10% with AEDs vs 13% without; p= .90). Class III data pertaining to metastases due to early study termination.
|
|
Glantz er al,8 1996
|
Single-institution, prospective, randomized controlled trial of VAL vs placebo pill for length of study in patients with cerebral metastases (lung, breast, melanoma).
Patients randomized within 14 days of diagnosis, and had no previous seizures, >1 supratentorial brain lesion, KPS ≥ 50%, and no previous anticonvulsant use or other brain disease.
74 total study patients enrolled, 57 with metastases (28 VAL, 29 placebo control).
|
III
|
Seizures occurred in 35% of all study patients treated with VAL and 24% of all patients in the placebo group (p= .3). Insufficient data published for subgroup analysis of patients with brain metastases (77% of total study patients). Class III data pertaining to metastases due to lack of subgroup analysis.
|
AED, Anti-Epileptic Drug; KPS, Karnofsky Performance Scale; PHT, Phenytoin; VAL, Valproate.
Subgroup analysis not possible for patients with metastases.
id="chapter8Table2"Table 2. Summary of published data on prophylactic seizure medications for post-craniotomy patients with brain metastases
|
Author, Year
|
Description of Study
|
Data Class
|
Conclusions
|
|
Ansari et al,10 2014
|
Single-institution, retrospective chart review of post-operative AED use vs no post-operative AED use in patients with cerebral metastases following initial craniotomy for tumor resection.
Patients with no previous seizures or use of AEDs.
202 total study patients, 86 with metastases (53 prescribed AEDs, 33 not prescribed AEDs).
|
III
|
Overall, 22.8% of patients had a post-operative seizure (median follow-up 321 days). Prophylactic AEDs with a 1.62 times increased chance of seizures (p = .2867). A total of 19% of patients with metastases experienced seizures. Insufficient data provided for metastases specific sub-group analysis. Class III data pertaining to metastases due to lack of subgroup analysis.
|
|
Wu et al,11 2013
|
Single-institution, prospective, randomized controlled trial of PHT for 7 days post-craniotomy vs no seizure prophylaxis (control) in patients with cerebral metastases undergoing craniotomy for tumor resection.
Patients were previously untreated (except WBRT >1 month prior), with cerebral metastases from systemic cancer (lung, melanoma, renal, breast, and other), ≥8 years old, with a KPS ≥70, and no prior seizures or solely posterior fossa tumors.
123 total study patients, 77 with metastases (39 PHT, 38 controls).
|
III
|
Trial terminated early based on a high probability of data insufficiency. No significant difference in seizure rate between PHT and control groups (15 vs 13%, p = 1.00). The majority of seizures occurred >30 days post-operatively, with no significant difference across treatment groups for early (≤30 days; 3 vs 5%, p = .62) or late (>30 days; 13 vs 8%, p= .71) seizures. Significantly more adverse events noted with PHT (18 vs 0%, p= .01). Class III data pertaining to metastases due to early study termination.
|
|
Franceschetti et al,12 1990
|
Single-institution, prospective, randomized controlled trial of post-operative AEDs (phenobarbital or PHT) vs placebo (control) in patients with cerebral metastases undergoing craniotomy.
Patients had supratentorial tumors and no previous seizures.
A total of 63 study patients (phenobarbital or PHT, n= 41) or no AED (n= 22), 13 with metastases (subgroup breakdown not provided).
|
III
|
Overall, early postoperative seizures occurred in 7% of the AED cohort and 18% of the non-AED cohort (p= .23). Late postoperative seizures occurred in 12% of the AED cohort and 21% of the non-AED cohort (p= .64). Insufficient data provided for metastases-specific sub-group analysis. Class III data pertaining to metastases due to lack of subgroup analysis.
|
AED, antiepileptic drug; KPS, Karnofsky Performance Scale; PHT, Phenytoin; WBRT, Whole brain radiation therapy.
REFERENCES
1. Gavrilovic IT, Posner JB. Brain metastases: epidemiology and pathophysiology. J. Neurooncol. Oct 2005;75(1):5-14.
2. You G, Sha Z, Jiang T. The pathogenesis of tumor-related epilepsy and its implications for clinical treatment. Seizure. Apr 2012;21(3):153-159.
3. Maschio M. Brain tumor-related epilepsy. Curr. Neuropharmacol. Jun 2012;10(2):124-133.
4. Eichler AF, Loeffler JS. Multidisciplinary management of brain metastases. The oncologist. 2007;12(7):884-898.
5. Shaw MD, Foy PM. Epilepsy after craniotomy and the place of prophylactic anticonvulsant drugs: discussion paper. J. R. Soc. Med. Apr 1991;84(4):221-223.
6. Mikkelsen T, Paleologos NA, Robinson PD, et al. The role of prophylactic anticonvulsants in the management of brain metastases: a systematic review and evidence-based clinical practice guideline. J Neurooncol. Jan 2010;96(1):97-102.
7. Forsyth PA, Weaver S, Fulton D, et al. Prophylactic anticonvulsants in patients with brain tumour. Can. J. Neurol. Sci. May 2003;30(2):106-112.
8. Glantz MJ, Cole BF, Friedberg MH, et al. A randomized, blinded, placebo-controlled trial of divalproex sodium prophylaxis in adults with newly diagnosed brain tumors. Neurology. Apr 1996;46(4):985-991.
9. Robinson PD, Kalkanis SN, Linskey ME, Santaguida PL. Methodology used to develop the AANS/CNS management of brain metastases evidence-based clinical practice parameter guidelines. J. Neurooncol. Jan 2010;96(1):11-16.
10. Ansari SF, Bohnstedt BN, Perkins SM, Althouse SK, Miller JC. Efficacy of postoperative seizure prophylaxis in intra-axial brain tumor resections. J. Neurooncol. May 2014;118(1):117-122.
11. Wu AS, Trinh VT, Suki D, et al. A prospective randomized trial of perioperative seizure prophylaxis in patients with intraparenchymal brain tumors. J. Neurosurg. Apr 2013;118(4):873-883.
12. Franceschetti S, Binelli S, Casazza M, et al. Influence of surgery and antiepileptic drugs on seizures symptomatic of cerebral tumours. Acta Neurochir. (Wien.). 1990;103(1-2):47-51.
13. Abramson JD, Rosenberg HG, Jewell N, Wright JM. Should people at low risk of cardiovascular disease take a statin? BMJ (Clinical research ed ). 2013;347:f6123.
14. North JB, Penhall RK, Hanieh A, Frewin DB, Taylor WB. Phenytoin and postoperative epilepsy. A double-blind study. J. Neurosurg. May 1983;58(5):672-677.
15. Gokhale S, Khan SA, Agrawal A, Friedman AH, McDonagh DL. Levetiracetam seizure prophylaxis in craniotomy patients at high risk for postoperative seizures. Asian. J. Neurosurg. Oct 2013;8(4):169-173.
Source: Neurosurgery, January 9, 2019